In late 2020, a converted van appeared in central Glasgow. Inside were clean needles, sterilising equipment, mirrors, “sharps bins” for the disposal of syringes, and supplies of the overdose reversal drug naloxone. There were also boxes containing protein bars, tea, blankets and a defibrillator, as well as two chairs and tables where injections could be prepared.
The van had been converted, and was being driven, by Peter Krykant – an ex-outreach worker with his own history of homelessness and injecting drug use. Frustrated with the fact that no overdose prevention centre (OPC) had yet opened in the city despite calls from the local NHS, he took the law into his own hands and, after a successful crowdfunding campaign, opened one independently.
OPCs are places where people can take illegally purchased drugs in a supervised environment, using clean equipment and with staff able to intervene in the case of an overdose. The first such centre opened in the Swiss capital Bern in 1986, and there are now around 200 across the world from Berlin, Paris and Geneva to Sydney, Vancouver and New York.

Iain Masterton/Alamy
While the centres go under an array of different names including “drug consumption rooms”, “safer consumption sites” and “safe injecting facilities”, the essential concept – providing a safe environment for the use of risky, illegal drugs – remains the same. There have been no recorded overdose deaths within any of these centres since the first opened 36 years ago.
No such services exist in the UK, however. As drug-related deaths continue to rise, the debate over whether this should change has become increasingly heated – especially in Scotland, where drug mortality rates are among the highest in the world. The largest outbreak of HIV in the UK in over 30 years has been among people who inject drugs in Glasgow, Scotland’s largest city, and is ongoing.
Krykant’s unsanctioned Glasgow OPC operated for nine months. It oversaw 894 injection events involving heroin and cocaine and treated nine potentially fatal overdoses. Krykant describes its impact as “overwhelming”:
I saw people move from groin injecting to injecting in less dangerous areas [of the body] due to having a warm and well-lit environment where they could take their time and not feel rushed. Myself and the other volunteers who helped run the service witnessed people feeling cared about for the first time. The service turned into a beacon of safety for many. We started supplying basic things like warm clothing, drinks and sanitary products. On one occasion, we bought a wheelchair for a person who had lost a leg.
The Glasgow police largely tolerated the facility, although on one occasion Krykant was cautioned for refusing to let officers into the van while it was being used. And the media were fascinated: during its brief time of operation, reports about the van appeared in UK and international media including the New York Times.
Due to health issues, Krykant reluctantly closed the facility in the summer of 2021. The van was donated to the Transform Drug Policy Foundation and now tours the UK, demonstrating what an OPC would look like in practice. Krykant believes it served a vital purpose in demonstrating that “it could be possible to set up and run OPCs within current frameworks”. He is still hopeful that a formal facility will be commissioned in the near future – but the UK government remains opposed to their introduction.

Campaigning amid controversy
Pat Hudson is an emeritus professor of history at Cardiff University. In 2017, her son Kevin was found dead in a locked toilet in a department store in the Welsh town of Carmarthen. He was 32 and an experienced tree surgeon.
Kevin Hudson died of cardiac arrest and brain damage after injecting heroin. He had been battling addiction and was making progress, but died alone after the kind of accidental overdose that kills thousands of people in the UK every year. According to his mother:
If Kevin had had somewhere safe to go in the town to inject, without fear of criminalisation or stigma and with a medically qualified person in attendance, he would certainly not have locked himself in a toilet where no one could reach him.

Hudson, a member of the campaign group Anyone’s Child: Families for Safer Drug Control, is calling for OPCs to be introduced as a way of providing this kind of life-saving support. While first and foremost about saving lives, she says this is also about “providing medical and addiction advice for those seeking help”.
OPCs have been found to successfully reduce the risk of blood-borne virus transmission, signpost clients to treatment services, provide advice on safer consumption, and reduce levels of public injecting and discarded needles. By creating a non-stigmatising environment, they can also attract people who might otherwise not come into contact with support services – or who previously had unhappy experiences in treatment.
Another new high for drug deaths in England and Wales – here’s what needs to change
More than 300,000 people are thought to use opiates or crack cocaine regularly in England, of whom about half are in treatment. But even for those accessing such services, treatment can only help if they are kept safe and alive when they are using. For people such as Kevin Hudson, a lack of safe drug consumption spaces significantly increases the risk of death.
In December 2021, in response to record levels of drug-related deaths, the UK government committed more than £700m to improving treatment services in England and Wales – a desperately needed injection of money following years of disinvestment. But despite organisations such as the harm reduction charity Cranstoun signalling their intention to open OPCs when conditions allow, there are no plans for piloting such facilities in the UK government’s ten-year drug strategy for England.
Deaths related to drug poisoning in England and Wales:
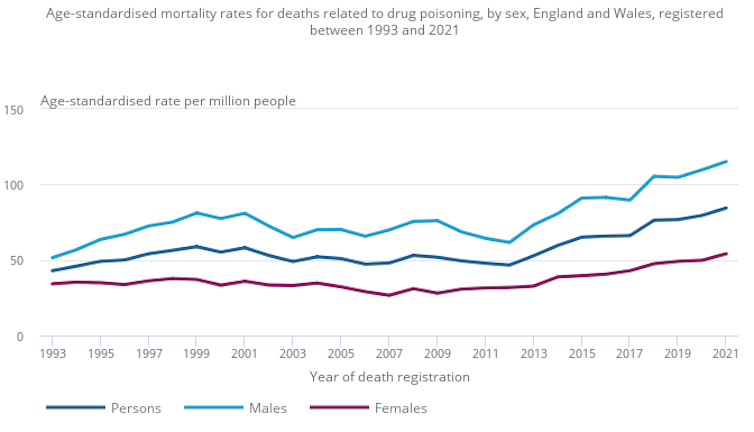
Office for National Statistics, CC BY
The UN’s International Narcotics Control Board has stated that OPCs are consistent with international drug control treaties, as long as they are part of a wider system of drug treatment. But under UK law, allowing the preparation of illicitly purchased drugs for ingestion could be construed as illegal.
As things stand, this means anyone operating an OPC could potentially be liable for prosecution. In 2016, Scotland’s largest NHS organisation, Greater Glasgow and Clyde, recommended that an OPC be opened in Glasgow city centre in response to the high rates of drug-related deaths and the emergence of an HIV outbreak, highlighting “widespread support [among] stakeholders from the target population, health services, and organisations representing drug users and their families”.
The lord advocate, Scotland’s chief public prosecutor, was asked to produce a “letter of comfort” to guarantee such facilities would not be a subject for prosecution. This proposal was not successful and the current lord advocate has stated she cannot make an activity unlawful, nor grant immunity from prosecution. However, in 2021 she said she “would be prepared to consider any such future proposal, but it would have to be specific and underpinned by evidence, and it would require fresh consideration”.

This story is part of Conversation Insights
The Insights team generates long-form journalism and is working with academics from different backgrounds who have been engaged in projects to tackle societal and scientific challenges.
In September 2021, the Scottish Drug Deaths Taskforce asked the Scottish government to “explore all options within the existing legal framework” that would enable OPCs to be piloted. Many Scottish MPs and MSPs have also called for action, with a private members’ bill currently being put through the Scottish parliament. And in January 2022, the UK Faculty of Public Health published a letter signed by every royal medical college calling on the UK government to “take steps towards funding [OPC] pilots … to save lives and reduce harm”. Scotland’s minister for drugs confirmed in June 2022 that a new proposal had been submitted for consideration by the Crown Office.
The UK government’s consistent refusal to introduce legal reforms to protect OPC providers from the threat of criminal sanctions has set Westminster against the Scottish government, which views OPCs as an important tool in its broader public health-led response to drug harms.
Recognising that a policy change in Westminster looks unlikely in the short term, the Scottish minister for drugs, Angela Constance, said the Scottish government is “leaving no stone unturned to deliver clinically and legally safe consumption facilities”. In contrast, according to Hudson, the UK government is “digging its heels in” because OPCs are seen as condoning illegal drug use. She explains:
There is a public health crisis with drug mortality which must be tackled … There needs to be a change of mindset among politicians so that they see public health policies on illicit drug consumption as a vote winner. The general public are mostly ready for this – it would not be hard to sell.
What the evidence tells us about OPCs
Insite was the first sanctioned and supervised injecting site to open in North America. Founded in 2003, it operates in the Downtown Eastside neighbourhood of Vancouver, a city that for decades has experienced high levels of homelessness, street injecting and drug-related deaths.
The Insite facility provides an array of booths, each with a table, mirror and waste bin. According to 2019 data, there is space for more than 300 injections a day. People need not be registered and there is no form-filling on arrival. In almost two decades, there have been thousands of overdose events but no fatalities.

Insite also offers a key source of evidence on the effectiveness and impact of OPCs. A 2011 study published in the Lancet found that, in the two years after Insite opened, the rate of overdose deaths within 500 metres of the facility fell by 35%, compared with 9% in the rest of Vancouver. More recently, a six-year cohort study found that people who used Insite and other OPCs in Vancouver at least weekly were almost 50% less likely to die of any cause than other people regularly using drugs.
Evidence from Insite and other established OPCs shows that these centres reduce risky activities such as needle sharing while increasing engagement with health and treatment services. This led the UK government’s Advisory Council on the Misuse of Drugs to call for them to be considered for the UK in 2016.
Similarly, a 2019 review of global evidence commissioned by Public Health England found that OPCs were effective in reducing high-risk injecting behaviours, drug-related litter and ambulance callouts while increasing access to education and other forms of social support. This review also confirmed there was no evidence of increased crime in the vicinity of OPCs.
Over the three decades since the first facility opened in Bern, the number of lives saved in OPCs across the world is likely to be enormous. And crucially, people who use drugs say they are likely to use OPCs if they are made available.
‘Absolute and utter hope’
Over a six-month period, our research team spoke to senior figures throughout Scotland – from the government and the criminal justice system to local health and social care teams and charities – to explore their views on OPCs and what they saw as barriers to adoption.
We also spoke to family members of people who use drugs, most of whom were overwhelmingly supportive. Many suggested that OPCs could provide a lifeline where other interventions had failed – and above all, “hope, just absolute and utter hope” that their loved ones could be kept safe when facing their most difficult and dangerous moments.
Many were bewildered as to why OPCs had not been introduced already. One family member described a “lightbulb moment” when she found herself thinking: “I can’t believe we don’t do this as a humane society.” Another asked: “Why would we not want to keep everybody safe?”
Scotland won’t prosecute personal possession of class A drugs, but outdated laws prevent deeper reforms
As well as recognising the lifesaving potential of OPCs, local decision makers highlighted their value in reducing levels of public injecting and discarded needles – often the main concern for the general public who, as one respondent put it, just “want rid” of drug problems in their area. Among decision makers and family members alike, OPCs represented a compassionate, non-judgmental approach to drug issues. They mattered not only because they could save lives, but because they stood for an alternative response to drug problems more broadly. As one family member put it:
By creating these drug consumption rooms, what we are really saying is: “We have an issue as a society – and it’s our responsibility to look after these people.”
Krykant, the pioneer of Glasgow’s mobile OPC van, sees this as a key point in understanding the full value of OPCs, concluding: “Although all data gathered is important, the human factor builds the most compelling case for implementation of these services.”
So why the resistance to introducing OPCs?
In June 2022, Alexis Goosdeel, director of the EU’s leading illicit drugs authority, described OPCs as “key instruments” in reducing drug harms. Goosdeel’s comments reflect a broad consensus within the drug research community – but this view is not shared by everybody.
The UK government argues that evidence of the effectiveness of OPCs is not sufficient to justify their introduction. In part, as one major review noted in 2018, this is because “estimating the overall effect of [OPCs] on fatal and nonfatal overdoses is difficult”.
Preventing individual deaths does not automatically mean overall drug mortality rates will be reduced. Someone who has had an overdose reversed in an OPC may still suffer a fatal overdose later in another location. And OPCs often operate alongside other services such as the provision of take-home naloxone and drug treatment services such as methadone, which significantly reduce death rates.
A recent review of an OPC in Melbourne, Australia, estimated that, of the 271 “extremely serious overdoses” that were treated in its first two years of operation, between 21 and 27 deaths were avoided. But again it is difficult to isolate the impact on drug deaths from other factors; some have argued that a “heroin drought” skewed the initial results from Sydney’s Medically Supervised Injecting Centre.

Taken alongside the practical difficulties of gathering data on people who are often hard to engage with, OPCs are not practical or ethical for the randomised controlled trial (RCT) or large-scale cohort evaluations that may be expected for other medical interventions – although a recent French study applied some of these methods and shown positive results. However, as a recent Lancet commentary on OPCs pointed out, “many public health interventions have been introduced without RCTs when their mechanism of action is clearly understood”.
Our study found that local decision makers are most concerned about whether OPCs are cost-effective compared with other interventions. Here, the question of how to interpret the available evidence – and decide what type of evidence is needed to justify investment – takes centre stage.
While the UK government points to a lack of RCT evaluations, local decision makers are more pragmatic. Although there was a recognition that politically, the evidence would need to be extremely strong to get the green light, it was felt that such evidence could be produced through pilots or studies from other countries, people with experience of drug use, and public perceptions. Most of those we interviewed in Scotland felt the available evidence was sufficient to move forward to implementation.
But anyone hoping to develop local evidence faces a Catch-22. Building evidence requires opening an OPC – yet this is blocked by the UK government on the grounds that the available evidence is insufficient. Without the reassurance of central government support or formal agreements with local police, many local authorities and service providers lack the confidence to go ahead.
What do families and communities want?
[When] she is living with you and she wakes up and she’s shaking and she is dreadful, you can say: “Do you want me to take you to the consumption room?” Hope … that’s all you are left with in the end. Hope that one day they say: “I don’t want to live like this anymore.” (Mother of a person who uses drugs)
Among the family members we interviewed, OPCs were attractive not only because of the evidence that they save lives, but because they gave new hope and the promise of greater dignity for their loved ones:
[An OPC] lends itself to people being given just a bit of space to say: “Actually I would want to do something different here.” I think it’s the gap between what we say and what we do at a deeply compassionate level. It’s easier to blame and shame and stigmatise people and see them as less than human, rather than see them as your own son, daughter, niece, nephew or uncle.
Communities affected by visible public drug consumption, however, often have different priorities. As a number of our participants pointed out, OPCs also need the support of these wider community members if they are to be successful.
In the past, community support for OPCs has often been strongest when large-scale drug scenes – such as emerged in parts of Germany and Switzerland in the 1980s and in Sydney in the 1990s – became a pressing social problem. More recently, the dramatic rise in UK drug deaths has raised the political pressure for action. However, public concern over visible drug consumption, especially when many people find it threatening or morally wrong, does not necessarily translate into support for OPCs.
A US survey found that many people believed money spent on OPCs would be better allocated to more conventional treatment and recovery programmes. Some community groups have expressed concern that OPCs would create a “honeypot effect”, not only attracting people using drugs but also dealers to the vicinity. However, other research suggests that if people hear stories about the experiences of people who use OPCs (or their families), rather than just being presented with statistics and data, then support increases.
A medically supervised injection facility matters for Victoria – and for more inclusive mental health support
When a proposal to open an OPC in the Richmond district of Melbourne was announced in 2017, there was widespread opposition from residents who feared it would encourage higher levels of drug use, increase crime, and attract more dealers to their areas. A later evaluation found that, while a large number of deaths had been prevented and ambulance callouts had fallen by 25% near the facility, some local residents reported no perceived change to factors such as the number of discarded needles – and a degree of opposition to the OPC remained.
But this was in stark contrast to the experience in Sydney. In 2010, ten years after its OPC opened, the amount of street injecting reported by residents had halved, and there was a “considerable reduction” in reported levels of discarded needles in the vicinity – leading to high levels of local support. The Insite centre in Vancouver also continues to enjoy high levels of public support for similar reasons.
In a recent UK-wide poll, just under half the respondents supported OPCs and only 18% opposed their introduction. Yet for some sceptics, the basic principle of facilitating drug consumption is wrong, especially without a clear requirement that visitors take steps towards recovery.
Under former prime minister Boris Johnson, the UK’s Conservative government argued that OPCs ran counter to their “tough” approach to drugs – not only enabling but even “encouraging use” (a claim not supported by any available evidence). Because it is much easier not to open an OPC, political inertia and institutional risk-aversion are always liable to prevent innovation.
Settling these controversies is about more than just appealing to evidence. Recent research confirmed what, to a casual observer, may seem obvious: even what you call these centres makes a difference. The label “drug consumption room”, for example, garners less public support than “overdose prevention centre” because one sounds like a facility designed to enable drug use to take place while the other frames it as saving lives. Getting public clarity on what OPCs actually do is therefore critical.
That OPCs save individual lives is beyond dispute. But they do so by accepting that creating safer environments for otherwise high-risk forms of drug consumption can be the right thing to do in certain circumstances. For some people, that will never be an acceptable principle – and the high level of stigmatisation towards people who inject drugs in political discussions only serves to reinforce this view. For many others, however, it sits at the heart of a compassionate and effective approach to reducing drug harms.
Will OPCs happen in the UK?
While every participant in our research supported piloting OPCs in principle, almost all decision makers felt the power to give the green light lay elsewhere. In Scotland, the issue is seen to have been kicked around like a political football, while the UK government insists that OPCs are a distraction from other treatment responses and claims advocates view them as a kind of silver bullet (something our participants strongly disputed).
Despite many expert voices arguing that after more than 50 years, a review of the UK’s primary drug legislation, the 1971 Misuse of Drugs Act, is urgently needed, it seems unlikely that this act will be amended in the short term at least. Senior police authorities (such as regional police and crime commissioners in England), however, could agree to memorandums of understanding, guaranteeing that local police will not enforce the act in ways that prevent OPCs from operating. This would be possible without any change to primary legislation but relies on senior local leaders championing their case.
There is certainly growing support for OPCs in English regions such as the West Midlands that have pressing drug problems. Should regional police forces arrive at agreements to allow local adoption, there are organisations ready to create facilities and a considerable body of evaluation literature to support effective service designs. Importantly, there are also researchers in place to ensure that new services are rigorously evaluated.
OPCs can only ever be one part of society’s response to drug dependency and harm. But without the opportunity to pilot them locally in the UK, it will never be possible to assess what the scale of that contribution could be, or how many lives would be saved. In the face of a growing drug death crisis, the need for action is more urgent than ever.

For you: more from our Insights series:
To hear about new Insights articles, join the hundreds of thousands of people who value The Conversation’s evidence-based news. Subscribe to our newsletter.




