The United States’ Centers for Disease Control and Prevention (CDC) has issued a health alert after the first case of H5N1 avian influenza, or bird flu, seemingly spread from a cow to a human.
A farm worker in Texas contracted the virus amid an outbreak in dairy cattle. This is the second human case in the US; a poultry worker tested positive in Colorado in 2022.
The virus strain identified in the Texan farm worker is not readily transmissible between humans and therefore not a pandemic threat. But it’s a significant development nonetheless.
Some background on bird flu
There are two types of avian influenza: highly pathogenic or low pathogenic, based on the level of disease the strain causes in birds. H5N1 is a highly pathogenic avian influenza.
H5N1 first emerged in 1997 in Hong Kong and then China in 2003, spreading through wild bird migration and poultry trading. It has caused periodic epidemics in poultry farms, with occasional human cases.
Influenza A viruses such as H5N1 are further divided into variants, called clades. The unique variant causing the current epidemic is H5N1 clade 2.3.4.4b, which emerged in late 2020 and is now widespread globally, especially in the Americas.
In the past, outbreaks could be controlled by culling of infected birds, and H5N1 would die down for a while. But this has become increasingly difficult due to escalating outbreaks since 2021.
When should we worry about bird flu making us sick? When we see human-to-human transmission – and there’s no evidence of that yet
Wild animals are now in the mix
Waterfowl (ducks, swans and geese) are the main global spreaders of avian flu, as they migrate across the world via specific routes that bypass Australia. The main hub for waterfowl to migrate around the world is Quinghai lake in China.
But there’s been an increasing number of infected non-waterfowl birds, such as true thrushes and raptors, which use different flyways. Worryingly, the infection has spread to Antarctica too, which means Australia is now at risk from different bird species which fly here.
H5N1 has escalated in an unprecedented fashion since 2021, and an increasing number of mammals including sea lions, goats, red foxes, coyotes, even domestic dogs and cats have become infected around the world.
Wild animals like red foxes which live in peri-urban areas are a possible new route of spread to farms, domestic pets and humans.
Dairy cows and goats have now become infected with H5N1 in at least 17 farms across seven US states.
What are the symptoms?
Globally, there have been 14 cases of H5N1 clade 2.3.4.4b virus in humans, and 889 H5N1 human cases overall since 2003.
Previous human cases have presented with a severe respiratory illness, but H5N1 2.3.4.4b is causing illness affecting other organs too, like the brain, eyes and liver.
For example, more recent cases have developed neurological complications including seizures, organ failure and stroke. It’s been estimated that around half of people infected with H5N1 will die.
The case in the Texan farm worker appears to be mild. This person presented with conjunctivitis, which is unusual.
Food safety
Contact with sick poultry is a key risk factor for human infection. Likewise, the farm worker in Texas was likely in close contact with the infected cattle.
The CDC advises pasteurised milk and well cooked eggs are safe. However, handling of infected meat or eggs in the process of cooking, or drinking unpasteurised milk, may pose a risk.
Although there’s no H5N1 in Australian poultry or cattle, hygienic food practices are always a good idea, as raw milk or poorly cooked meat, eggs or poultry can be contaminated with microbes such as salmonella and E Coli.
If it’s not a pandemic, why are we worried?
Scientists have feared avian influenza may cause a pandemic since about 2005. Avian flu viruses don’t easily spread in humans. But if an avian virus mutates to spread in humans, it can cause a pandemic.
One concern is if birds were to infect an animal like a pig, this acts as a genetic mixing vessel. In areas where humans and livestock exist in close proximity, for example farms, markets or even in homes with backyard poultry, the probability of bird and human flu strains mixing and mutating to cause a new pandemic strain is higher.
Author provided
The cows infected in Texas were tested because farmers noticed they were producing less milk. If beef cattle are similarly affected, it may not be as easily identified, and the economic loss to farmers may be a disincentive to test or report infections.
How can we prevent a pandemic?
For now there is no spread of H5N1 between humans, so there’s no immediate risk of a pandemic.
However, we now have unprecedented and persistent infection with H5N1 clade 2.3.4.4b in farms, wild animals and a wider range of wild birds than ever before, creating more chances for H5N1 to mutate and cause a pandemic.
Unlike the previous epidemiology of avian flu, where hot spots were in Asia, the new hot spots (and likely sites of emergence of a pandemic) are in the Americas, Europe or in Africa.
Pandemics grow exponentially, so early warnings for animal and human outbreaks are crucial. We can monitor infections using surveillance tools such as our EPIWATCH platform.
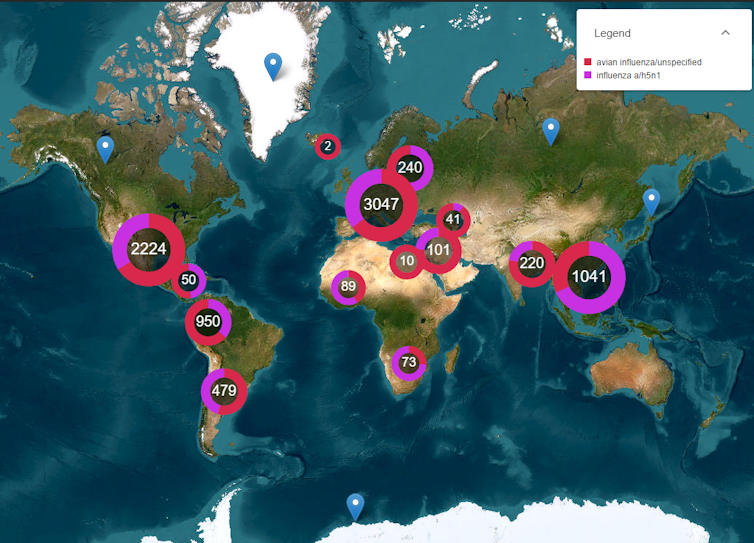
EPIWATCH/author provided
The earlier epidemics can be detected, the better the chance of stamping them out and rapidly developing vaccines.
Although there is a vaccine for birds, it has been largely avoided until recently because it’s only partially effective and can mask outbreaks. But it’s no longer feasible to control an outbreak by culling infected birds, so some countries like France began vaccinating poultry in 2023.
Migrating birds could bring lethal avian flu to Australia’s vulnerable birds
For humans, seasonal flu vaccines may provide a small amount of cross-protection, but for the best protection, vaccines need to be matched exactly to the pandemic strain, and this takes time. The 2009 flu pandemic started in May in Australia, but the vaccines were available in September, after the pandemic peak.
To reduce the risk of a pandemic, we must identify how H5N1 is spreading to so many mammalian species, what new wild bird pathways pose a risk, and monitor for early signs of outbreaks and illness in animals, birds and humans. Economic compensation for farmers is also crucial to ensure we detect all outbreaks and avoid compromising the food supply.




