It is a niche kind of membership that lets you in behind the doors of an acute mental health facility. Unless you work there or are admitted as an inpatient, these publicly funded private spaces that house people at their most vulnerable are really difficult to get into.
This makes them challenging to study and, without such research, challenging for architects to design well. We opened up the black box of acute mental health care facilities in New Zealand to understand their purpose, how people experience them and what informs their architectural design.
Design matters. Fit-for-purpose psychiatric facility design promotes better mental health and wellbeing. This is a no-brainer for people who work and stay in these units.
Unfortunately, the evidence base for the architectural design of acute mental health facilities has been haphazard, with costly implications.
To understand how these settings serve their populations and if we can do better, we studied four acute mental health facilities around New Zealand, looking at the old, the new and some in between.
We examined policy documents and architectural plans and made site visits to take photographs, conduct a building survey and interview staff, service users and visiting family members.
How psychological aspects of healing are important for hospital design
Not fit for purpose
In terms of the purpose of acute mental health facilities, we found confusion. Only one facility had a written model of care, which is the critical blueprint for architects to understand what and who they are designing for.
Fortunately, we did find consensus that the underpinning philosophy of care was the “recovery model”. We figured recovery principles, in concert with Indigenous Māori values and models of health and wellbeing, could and should inform the architectural blueprint for these buildings.
Ruby Crooks, CC BY-SA
A recovery-oriented environment suggests a design that fosters connection, hope, identity, meaning, empowerment and safety. This was not what we found.
While service users were relieved to get sleep, respite and diagnosis or treatment for their distressing symptoms and spoke highly of the staff compassion and quality of care, for many the acute mental health environment was confusing, frightening, disempowering, restrictive, boring and sometimes unsafe and traumatising.
Name in vain
In what feels like institutional gaslighting, the naming of these units is bewilderingly Kafkaesque. We found “open units”, the name given to lower-acuity facilities, typically have their doors locked. Given the voluntary status of some patients, this is counter intuitive.
Then there are the warm-fuzzy, therapeutic-sounding names for the prison-like seclusion wings, often with Indigenous Māori names, implying such spaces are peaceful retreats when inpatients felt they were anything but.
There is hope however. New Zealand has an aspirational goal of zero seclusion. Bafflingly, we are yet to build a facility without a seclusion wing.
Mind numbing
Service users talked about boredom in dilapidated, resource-scarce and low-stimulus environments. There was little to do in many of the wards and, while all had TVs and a few dog-eared books, activities and allocated spaces were often limited.
Often art rooms, sensory rooms and other occupational therapy spaces were locked and completely unused due to a lack of staff or the ability to supervise effectively.
Facility decision-making around recreation sometimes appeared dubious. Some had exercise bikes inappropriately located in the public reception, or a broken basketball hoop, and colouring-in and smoothie-making seemed central to some recreational programmes.
Lack of meaningful activities led some to start or restart smoking, which was the dominant activity observed in the internal ward courtyards, despite hospital smokefree polices. Fear of violence was cited as a major barrier to smokefree implementation.
Beds and meds
We were struck by the paucity of therapeutic options. While all units had occupational therapists, social workers and psychiatrists, the main treatment was medication, or as some staff described it, “beds and meds”.
Although many were grateful for medication, service users complained about the absence of talking therapies, lamented the lack of access to psychologists and many just wanted someone, anyone, to talk to. We found service users counselling each other.
We also found a lack of consideration of various gendered and cultural needs in the models of care, building design and layout. Shared bathrooms were described as “gross” and there were issues with acoustic and visual privacy.

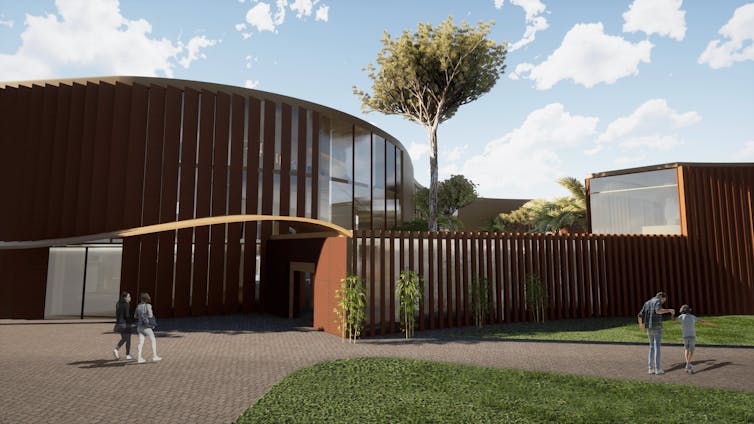
Ruby Crooks, CC BY-SA
Buildings and models of care did not accommodate or consider Māori values and cultural practices well, although New Zealand’s newest facility, Tiaho Mai in Auckland, boasts bi-cultural features due to co-design with Māori.
At a time when evidence suggests a more “domestic” look and feel of acute mental health care buildings would be more therapeutic, New Zealand’s facilities are more hospital-like or institutional than those in the UK.
Design makes a place a prison or a home. Turning ‘human-centred’ vision for aged care into reality
Courtyards, critical in locked facilities to access fresh air, sunshine and nature, were also institutional, often no more than a concrete pad with little to no nature. They failed to provide any real therapeutic value.
There were some positives though. Encouragingly, many staff told us, despite all the challenges associated with working in these settings, they stayed because the work was interesting, they loved the people and enjoyed that their work made a difference to people’s lives.
How we can do better
The current model and buildings are not serving people well. While the prospect of bulldozing the current stock might appeal, without places to safely care for people experiencing profound mental distress, our most vulnerable may find themselves dislocated from their homes and communities, or worse, in the criminal justice system.
We should and are making improvements to our existing stock of buildings, and some are being totally rebuilt. In the interim, small changes to these environments to foster more inpatient autonomy can be made, including self-locking bedroom doors, built-in privacy controls and the provision of lockers to store valuables.
Your home, office or uni affects your mood and how you think. How do we know? We looked into people’s brains
However, a more profound transformation around the model of care itself is required. Fortunately, a major paradigm shift towards alternative models of acute mental health care is brewing. Many countries, including New Zealand, are re-examining care provision with a human rights lens.
We need to work together to re-create a mental health system that reflects values of human rights, autonomy and person-centred practice and aligns with the rights of Indigenous people. We need a suite of options and new models of mental health care to provide the blueprints for our architects to design and upgrade our places of care.




