Opioid drugs such as morphine and fentanyl are like the two-faced Roman god Janus: The kindly face delivers pain relief to millions of sufferers, while the grim face drives an opioid abuse and overdose crisis that claimed nearly 70,000 lives in the U.S. in 2020 alone.
Scientists like me who study pain and opioids have been seeking a way to separate these two seemingly inseparable faces of opioids. Researchers are trying to design drugs that deliver effective pain relief without the risk of side effects, including addiction and overdose.
One possible path to achieving that goal lies in understanding the molecular pathways opioids use to carry out their effects in your body.
How do opioids work?
The opioid system in your body is a set of neurotransmitters your brain naturally produces that enable communication between neurons and activate protein receptors. These neurotransmitters include small proteinlike molecules like enkephalins and endorphins. These molecules regulate a tremendous number of functions in your body, including pain, pleasure, memory, the movements of your digestive system and more.
Opioid neurotransmitters activate receptors that are located in a lot of places in your body, including pain centers in your spinal cord and brain, reward and pleasure centers in your brain, and throughout the neurons in your gut. Normally, opioid neurotransmitters are released in only small quantities in these exact locations, so your body can use this system in a balanced way to regulate itself.
The problem comes when you take an opioid drug like morphine or fentanyl, especially at high doses for a long time. These drugs travel through the bloodstream and can activate every opioid receptor in your body. You’ll get pain relief through the pain centers in your spinal cord and brain. But you’ll also get a euphoric high when those drugs hit your brain’s reward and pleasure centers, and that could lead to addiction with repeated use. When the drug hits your gut, you may develop constipation, along with other common opioid side effects.
Targeting opioid signal transduction
How can scientists design opioid drugs that won’t cause side effects?
One approach my research team and I take is to understand how cells respond when they receive the message from an opioid neurotransmitter. Neuroscientists call this process opioid receptor signal transduction. Just as neurotransmitters are a communication network within your brain, each neuron also has a communication network that connects receptors to proteins within the neuron. When these connections are made, they trigger specific effects like pain relief. So, after a natural opioid neurotransmitter or a synthetic opioid drug activates an opioid receptor, it activates proteins within the cell that carry out the effects of the neurotransmitter or the drug.
Opioid signal transduction is complex, and scientists are just starting to figure out how it works. However, one thing is clear: Not every protein involved in this process does the same thing. Some are more important for pain relief, while some are more important for side effects like respiratory depression, or the decrease in breathing rate that makes overdoses fatal.
So what if we target the “good” signals like pain relief, and avoid the “bad” signals that lead to addiction and death? Researchers are tackling this idea in different ways. In fact, in 2020 the U.S. Food and Drug Administration approved the first opioid drug based on this idea, oliceridine, as a painkiller with fewer respiratory side effects.
However, relying on just one drug has downsides. That drug might not work well for all people or for all types of pain. It could also have other side effects that show up only later on. Plenty of options are needed to treat all patients in need.
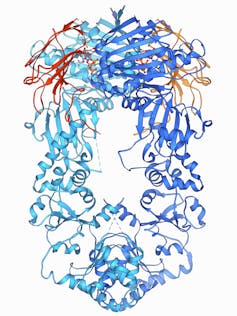
Laguna Design/Science Photo Library via Getty Images
My research team is targeting a protein called Heat shock protein 90, or Hsp90, which has many functions inside each cell. Hsp90 has been a hot target in the cancer field for years, with researchers developing Hsp90 inhibitors as a treatment for many cancer types.
We’ve found that Hsp90 is also really important in regulating opioid signal transduction. Blocking Hsp90 in the brain blocked opioid pain relief. However, blocking Hsp90 in the spinal cord increased opioid pain relief. Our recently published work uncovered more details on exactly how inhibiting Hsp90 leads to increased pain relief in the spinal cord.
Our work shows that manipulating opioid signaling through Hsp90 offers a path forward to improve opioid drugs. Taking an Hsp90 inhibitor that targets the spinal cord along with an opioid drug could improve the pain relief the opioid provides while decreasing its side effects. With improved pain relief, you can take less opioid and reduce your risk of addiction. We are currently developing a new generation of Hsp90 inhibitors that could help realize this goal.
There may be many paths to developing an improved opioid drug without the burdensome side effects of current drugs like morphine and fentanyl. Separating the kindly and grim faces of the opioid Janus could help provide pain relief we need without addiction and overdose.




