Ontario’s Minister of Sport, 71-year-old Neil Lumsden, recently announced his decision to donate his brain to the Concussion Legacy Foundation Canada to support research on brain injuries.
Lumsden played 10 years in the Canadian Football League, winning four Grey Cups and while he knows he had his “bell rung” a number of times during his career, he doesn’t believe he has had any long-term neurological damage. Helping researchers find out why his brain seems to be more resilient than some of his teammates motivated his decision.
As if on cue, on Sept. 24, 54-year-old National Football League Hall of Famer Brett Favre revealed during unrelated testimony before the United States congress that he had been diagnosed with Parkinson’s disease, likely as a result of hundreds of concussions experienced during his storied career.
Why have these two athletes had such different outcomes?
Assessing and managing concussion
While we have some tools to assess and manage concussions at the acute phase, we don’t have much at our disposal to monitor long-term progression. In the acute phase, concussions are not visible on conventional MRI or CT scans. This is one of the reasons a concussion is also called a “mild” traumatic brain injury (mTBI). Such scans are only sparingly used to rule out more severe TBI consequences such as brain bleeds.
(AP Photo/Mark Schiefelbein)
While there are some potential blood-based biomarkers for diagnosing acute concussion, there are very few broadly accessible tools to study the long-term biological effects on brain cellular and molecular function. These functions likely govern an individual’s trajectory towards neurodegeneration, a journey that can take years or decades.
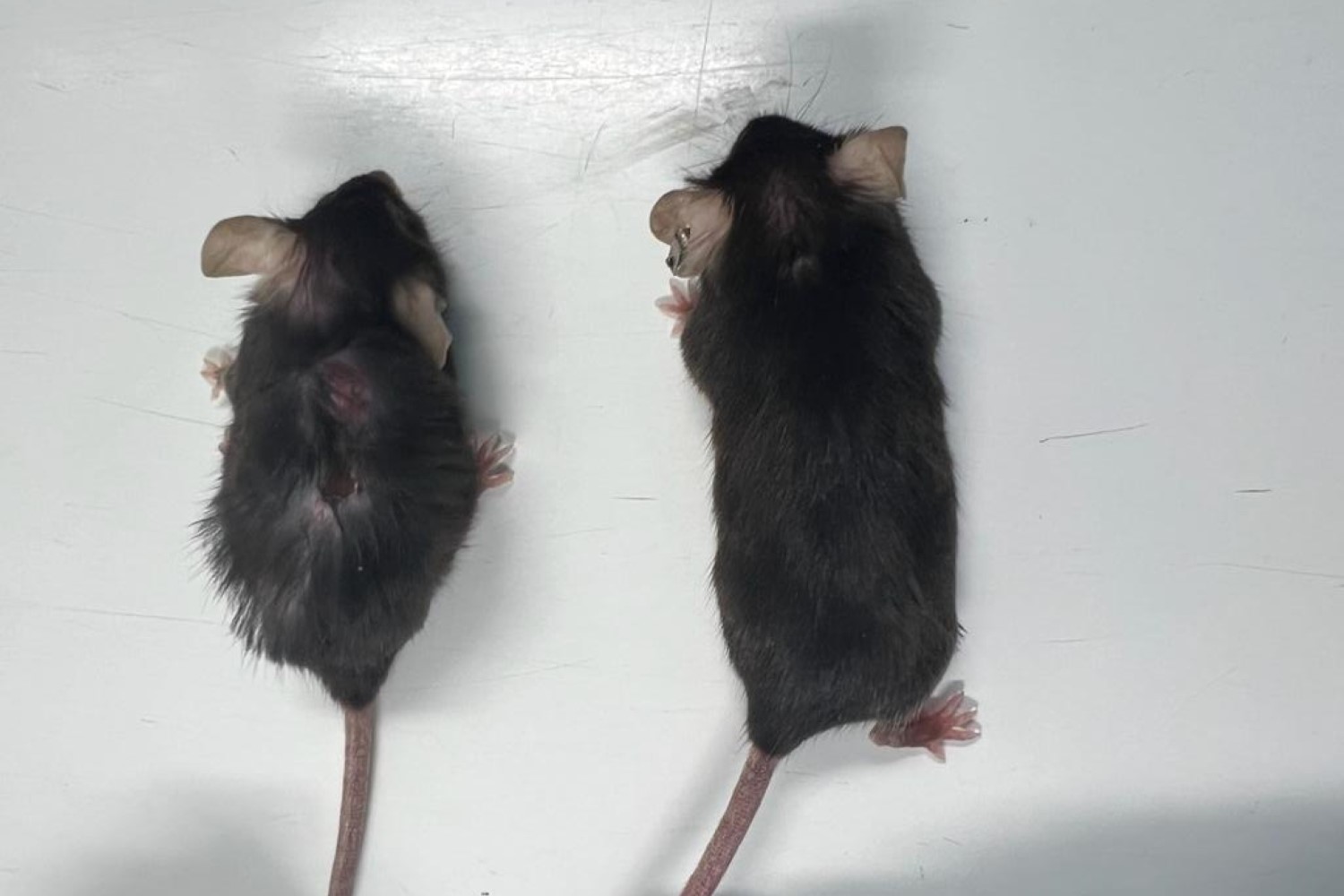
The risk of neurodegeneration — a progressive loss of structure or function of neurons — increases with the frequency and severity of concussions. An individual does not even have to be concussed for brain damage to be observed. Repeated subconcussive impacts have been shown by the group I work with at the Centre for Functional and Metabolic Mapping and others to produce persistent changes in brain structure and function in young female athletes as well as in blood biomarkers in young male athletes.
Both these studies used more sophisticated MRI approaches, including resting-state functional MRI which reveals how brain areas communicate with each other, and diffusion tensor imaging that measures the physical integrity of the connections between brain areas.
Fortunately, we think most of the study subjects will not go on to develop neurodegenerative disorders, but we don’t understand why some like Favre do and others like Lumsden don’t.
From human and animal studies, we do understand some of the major biological consequences of head impacts that may pave the way for neurodegeneration. Chronic inflammation has been linked to the development of neurodegenerative diseases, like Alzheimer’s disease and Parkinson’s disease, where neurons progressively die.
Tau protein tangles disrupt the normal functioning of neurons and are one of the hallmark features of Chronic Traumatic Encephalopathy (CTE), a neurodegenerative disease linked to repeated head injuries. CTE is known to cause memory loss, confusion, impaired judgment, impulse control problems, aggression and eventually dementia. CTE can be present in the brains of people who had repeated hits, but never had a diagnosed concussion, such as former Penn football captain Owen Thomas.
CTE often is observed in younger populations (like Thomas) but can only be diagnosed postmortem. A recent survey in the NFL showed that one-third of retired players believe they have CTE based on symptoms, and almost 10 per cent already had a diagnosis of Alzheimer’s or other dementias. Subtle shearing or stretching of axons — the long, filament-like parts of neurons that carry signals between brain cells — can occur with impacts. Over time, damaged axons may degenerate, contributing to brain atrophy (shrinkage) and cognitive decline.
Our own research shows that the longer axon bundles that connect distant areas of the brain are damaged and that this damage can accumulate with each subsequent injury. Axons are the threadlike extensions of neurons that transmit electrical impulses between brain areas, often grouped together in bundles.
The brain is normally protected by a structure called the blood-brain barrier, which tightly regulates the entry and exit of metabolites and waste products in the brain. After one or more impacts, the blood-brain barrier can become damaged, allowing toxic proteins, chemicals and cells to infiltrate the brain. This can trigger a destructive cycle of inflammation and cell death, setting the stage for long-term neurodegeneration.
Many of these factors can be measured in research settings using positron emission tomography scans, or various advanced forms of MRI. Some of these may have predictive power for resilience in the future. Genetic predisposition may be important. People carrying the APOE4 gene or the alpha-synuclein Rep 1 promotor allele may be more at risk for Alzheimer’s or Parkinson’s, respectively, after repeated hits. Other studies have not found such a link.
It is clear that some brains are able to compensate at various levels. This process is likely linked to what is called cognitive reserve, which is the ability of a brain to maintain cognitive function in the face of advancing disease or injury. It has been linked to genetics, level of education, social interactions and health status. It likely depends on the brain’s ability to reroute information, much like a traffic detour — something we can measure with functional MRI. Patients with higher cognitive reserves have better postconcussive outcomes, at least in the short term.
A concussion might be considered a “mild” injury, but its effects can last a lifetime, especially when multiple impacts occur. This is why understanding concussions and their long-term effects is important for predicting who might suffer from neurodegeneration.