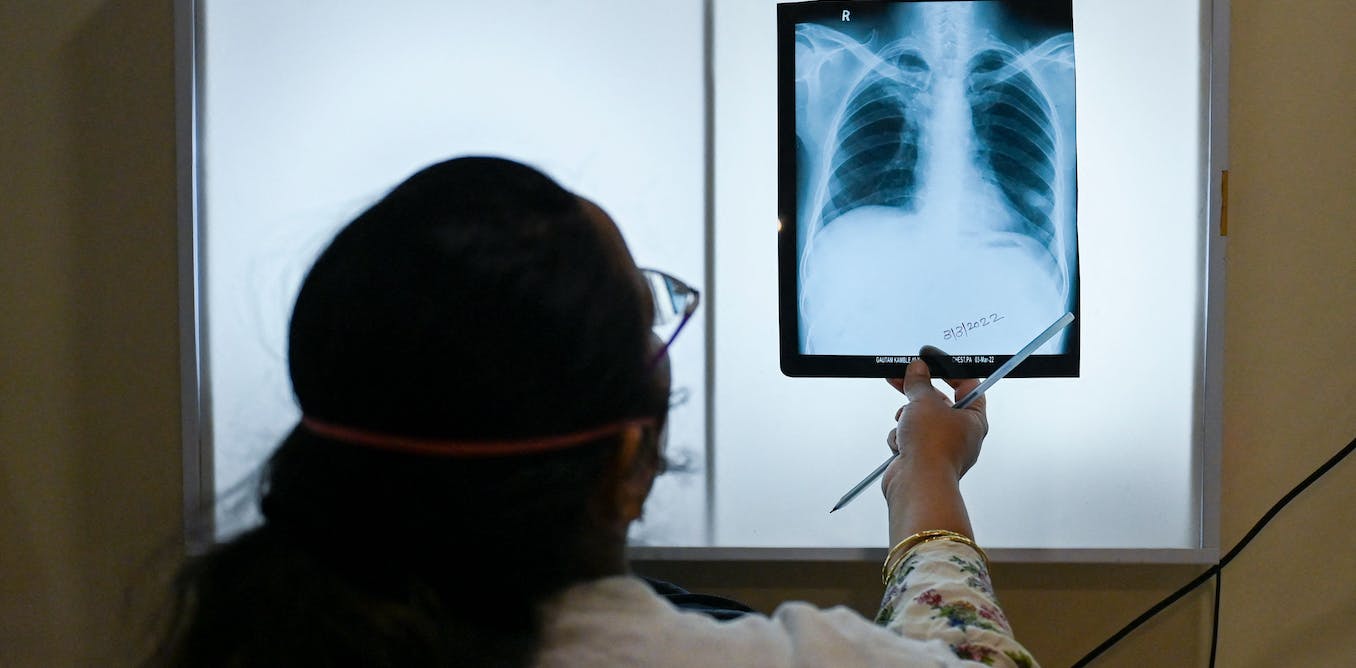
Tuberculosis (TB) is a preventable and curable disease. Half of the world’s 30 highest TB burden countries are in Africa. In many of these countries, TB is the leading cause of death across age groups, but especially among children. Globally, TB is the leading cause of death by any single infectious agent (above COVID-19 and HIV).
The people most affected by TB are often the most socio-economically marginalised, with the fewest reserves to take them through the treatment journey. This is extremely challenging, with complex, often delayed diagnosis, many months of treatment, and often long-term effects after treatment. The Conversation Africa’s Ina Skosana spoke to Graeme Hoddinott, a socio-behavioural science lead at the Desmond Tutu TB Centre, Stellenbosch University, and an African Academy of Sciences ARISE Fellow.
What’s the TB burden among young people?
In Africa, of the three million people who develop TB disease every year, nearly 160,000 are children 0-4 years old, and another 160,000 are 5-14 years old. Every year, about 500,000 people in Africa die because of TB. Children make up 15% (75,000) of these deaths.
Less than half of the children aged 0-14 who have TB are diagnosed – so they never even start treatment.
What are some of the drivers?
TB is transmitted between people through the air. When a person with TB coughs or breathes out, some of the TB bugs are expelled to float in the air. If someone else then breathes the bugs in, they cause a new infection. There are several factors that increase the risk of TB transmission. These include actions that increase the number of bugs in the air, such as not wearing a mask and coughing more. And actions that increase exposure, such as spending long periods of time breathing the air in.
A person might breathe the TB bugs in (that is, become infected), but not become ill. This is known as latent TB. Sometimes, though, the TB bugs are able to multiply and escape the body’s immune system. As the number of bugs increases, the person begins to experience symptoms such as coughing, drenching sweats and weight loss. This is then called TB disease.
A variety of factors increase the risk of progressing from TB infection to disease. These are factors that might impede the body’s natural immune functioning, such as undernourishment or smoking.
Children (especially young children) have less developed immune systems. This makes their chance of progressing from infection to disease higher than it is for adults.
Prevention of infection can be done through reducing risks of transmission, for example by opening windows to allow the bugs to blow away. Also, if a person with TB is on treatment, then the number of bugs they expel is dramatically reduced. That’s why it’s important to get an early diagnosis and start treatment.
Where there is an exposure risk, we can also use medicines to reduce the chance of developing disease – this is called TB preventive therapy. The most recent World Health Organization guidelines suggest that preventive therapy be offered to everyone who has significant exposure risk to an adult or adolescent with TB. For example, think about young children who are sharing a bed with their mother. If she has TB, then the child should be offered preventive therapy, as should other people who share their home.
Unfortunately, in most settings in Africa, implementation of TB preventive therapy is either non-existent or extremely sub-optimal. Historically, the only available TB preventive regimen was a once-daily treatment for six months that is burdensome to administer; new regimens are becoming available. Unfortunately, the limited resources available to TB services have prioritised TB treatment and not prevention.
Where are the gaps?
There have been substantial improvements in some areas of TB therapeutics, with shorter, more palatable regimens and more easy-to-use formulations. However, these are not universally available and are still not optimal. Even “shorter” treatment is four months long. Health systems are poorly equipped to support continuity of care when patients (including children and adolescents) move between facilities.
Far too many children who initiate both TB preventive therapy and TB treatment are lost to follow-up. TB programmes across the world have yet to operationalise the high-minded ideals of “patient-centred care”. The experiences of adolescents and young people (10-24 years old) accessing TB services are often especially problematic. For example, adolescents report being assumed to have HIV, being shouted at for being sexually active (even if they are not) and being told to access TB services at times when they are in school.
There is also limited integration between health services and other sectors (like basic education) to make care easier to get. There remain high rates of TB-associated stigma, and the costs of TB care (economic, social and psychological) can be catastrophic and long-lasting.
How must TB programmes be tailored?
A fraction of the funding and collective effort that was mobilised for COVID-19 could realistically push towards TB elimination. Perversely, instead, resources redirected towards COVID-19 have set the global TB programme back by a decade’s worth of progress.
TB programmes must be tailored by listening to the preferences and priorities of people affected by TB, by working to address the real-world limitations experienced by frontline health services, and by continuing to develop better, more acceptable therapeutics; especially medicines that are more acceptable for children and easier for caregivers to prepare and administer.
But really all of that can only make a big difference if we all wake up to this leading cause of death, especially among children, and care more.